Laparoscopic Davydov Neovagina
Drs. Moore and Miklos utilize the laparoscopic modification of the Davydov procedure to create vaginas in women born without them (i.e. MRKH syndrome/vaginal agenesis) or in women that have a shortened vagina or painful vaginal cuff following surgery (such as hysterectomy). They complete more laparoscopic vaginal and pelvic reconstructive surgeries at their center in Atlanta than any other in the US and are considered world leaders in the field. They have women travel to Atlanta for their surgeries from all over the US and are invited to lecture and operate on their techniques throughout the world. They have pioneered many procedures that are considered standard of care in the field of Urogynecology today and complete all their abdominal procedures laparoscopically (many of which are still done through large abdominal incisions at most other centers).
The Davydov Procedure is a surgical procedure used to create a full-length vagina in young women that are born without a vaginal canal or lengthen the vagina in women with surgically shortened or scarred down vaginas. It is one of the most successful procedures described for this condition and utilizes the patient’s own peritoneum (the cellular layer that lines the walls of the pelvis and the abdominal cavity) as the new vaginal canal. Dr. Miklos and Moore can use their expertise as laparoscopic pelvic/vaginal reconstructive surgeons to be able to complete the procedure laparoscopically, i.e. through tiny mini-incisions in the belly which makes it an outpatient type surgery. They operate from large Hi-def TV screens that magnify the field allowing them to complete the surgery with more precision, better visualization, less blood loss and less complications versus traditional surgery. Recovery is rapid and the procedure carries the lowest risk of scarring down or losing the length created than any other procedure described to create vaginal length.
MRKH Surgery: Laparoscopic Davydov Neovagina
Many surgeons use an open abdominal incision (laparotomy) to complete these types of procedures. Dr. Miklos and Dr. Moore complete the neovagina procedure laparoscopically. See their incisions ‘laparoscopic’ (small incision) versus others ‘laparotomy’ (big incision). Which would you rather have?
Surgical Procedure
Dr. Miklos and Moore utilize their standard approach to laparoscopic pelvic reconstruction for the Laparoscopic Neovagina. Tiny incisions are made in the belly (one is hidden in the belly button) to allow access to the abdominal cavity. The procedure is completed with both a vaginal and laparoscopic approach, i.e. work is done from below vaginally, as well as above in the abdomen through the scope. Dr Moore and Miklos have a dedicated team of assistants to allow them to work together to accomplish the procedure. In the traditional approach to the surgery, approximately half of it is completed vaginally, however secondary to their expertise, they can complete most of it laparoscopically. The procedure typically takes them approximately 1 to 2 hours to complete and is completed in an outpatient type hospital setting.
MRKH Neovagina Surgery Photos
Figure 1:
Demonstrates the laparoscopic view down into the pelvis. The shiny covering of the pelvis (called peritoneum) will become the lining of the new vaginal canal. The arrow and dotted lines depict where the top of the vagina or dimple is located and that is the area that will be opened under direct visualization at the beginning of the procedure.
Once abdominal access is obtained, the vaginal dimple (or top of scarred down vagina in a shortened vagina) is opened to start the procedure. The most flexible part of the top of the vagina or dimple is located and with direct visualization from above laparoscopically, the vagina is opened with a large enough opening to accommodate two to three fingers.
Figure 2:
Vaginal photo of a MRKH patient with normal appearing external vagina, however one can visualize the vagina is very shortened and just has a dimple where the vaginal canal should start. The dotted lines in the picture depict the incision that will be made to open up the top of the current vagina into the pelvis to enable the lengthening/neovagina procedure to be completed. The pelvic view of this incision can be seen above in Figure 1.
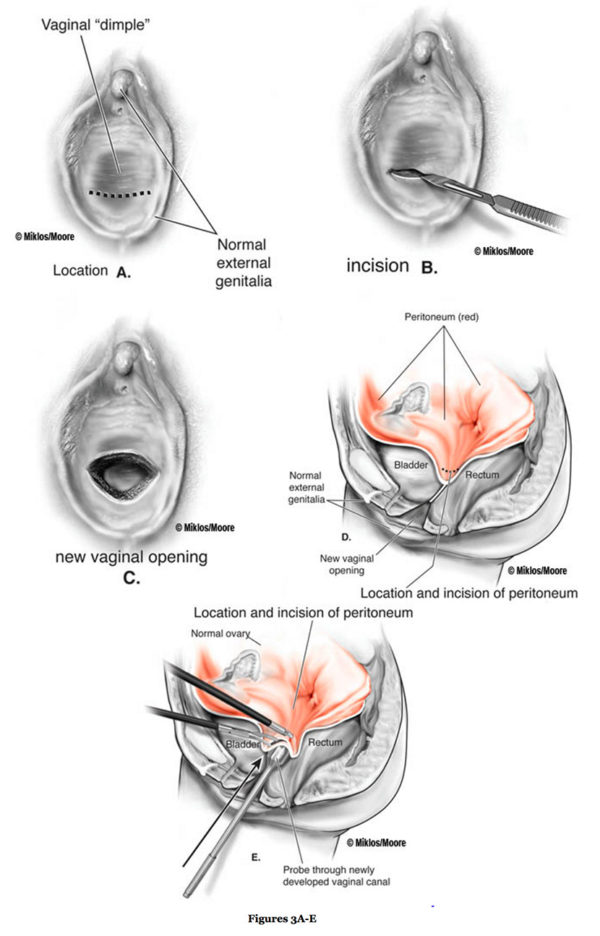
Figures 3A-E above:
The illustration (Figure 3 A-E) demonstrate where the incision is made in the vaginal dimple (becomes new vaginal opening) and then the probe is pushed up into the pelvis (Figure E) to incise the last layer (peritoneum).
Once the top of the vagina is opened into the pelvic cavity, the edges of the incised peritoneum is pulled down to the vaginal epithelium and the edges sutured together all around the opening. This is a step that can be completed vaginally, however Dr. Moore and Miklos typically will complete this step laparoscopically as well.
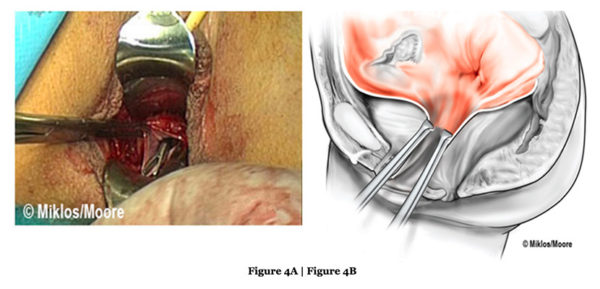
Figure 4A:
The edges of the peritoneum can be visualized and these are advanced down and sutured to the edges of the opened vaginal skin edges.
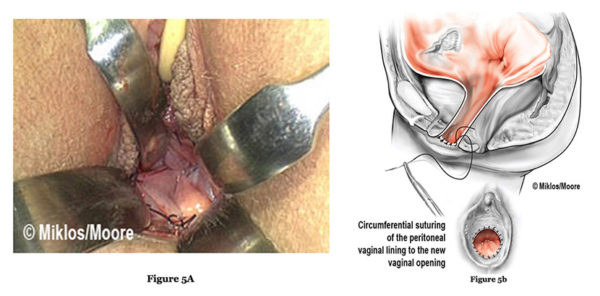
Figure 5A:
There are NO raw surface edges exposed (these can be seen in Figure 4A). They are covered with the suturing of the peritoneum edges to the vaginal edges all the way around the circumference of the vagina and this minimizes risks of the vagina scarring down. This picture shows the lining of the new vagina very well, again note how there are NO raw surfaces and the peritoneal lining is very smooth and already completely epithelialized, i.e. it is not like a skin graft that must heal or be accepted by the body.
The depth of the new vagina can be visualized in Figure 5B. Peritoneum sutured to vaginal epithiam (skin) as seen in Figure 5B.
The new top or apex (cuff) of the vagina is now created laparoscopically. The vaginal length is marked from below and the peritoneum up higher in the pelvis is sutured in a purse string fashion to create the new upper portion of the vagina. Care is taken to avoid the ureters (the tubes going from the kidneys to the bladder) as well as the bowel.
Purse string sutures gathering together pelvic peritoneum – creating new top of the vagina
Dr. Miklos & Moore can typically achieve a vaginal length between 9 to 11 cm with this technique.
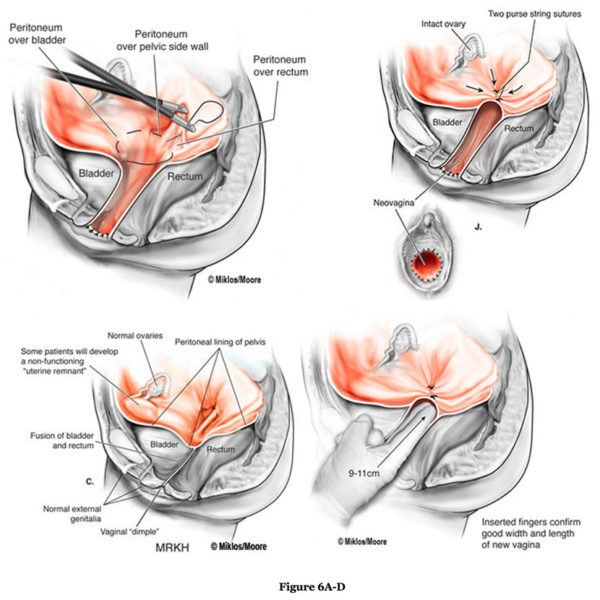
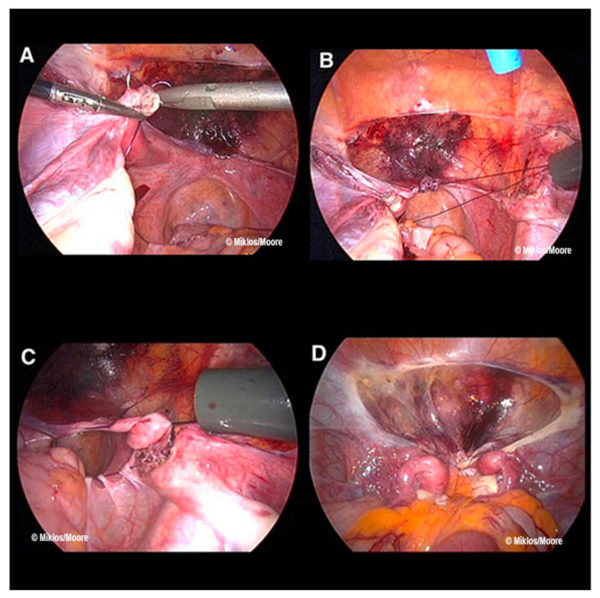
Figure 6(A-D):
Figure (A) and (B) show the beginning of the suture grasping the pelvic peritoneum just under the ovary and then continuing across the superior aspect which incorporates the bladder peritoneum (a releasing incision is made above this portion to allow this portion of the peritoneum to be more mobile). Figure (C) shows the suture going all the way around the peritoneum and one can visualize what will be the vaginal canal below the suture. When this suture is tied down (Fig. D), this becomes the top of the new vaginal canal. Drs. Moore and Moore can typically achieve a vaginal length of between 9 to 11 cm with this technique.
While no surgery is risk free, the risks of the laparoscopic neovagina technique that Dr. Miklos and Moore utilize are very minimal, especially when compared to other surgical techniques to create or lengthen the vagina. Other techniques, including the McIndoe procedure or procedures that utilize a piece of intestine to create the vagina can be much more invasive and carry much higher risks of bowel or bladder injury, infection, bowel obstruction or scarring down of the vaginal canal post-operatively. The Laparoscopic Neovagina approach utilizing peritoneum results in a vaginal canal that has minimal risks of scarring down and has success rates of over 97% a fully functional vagina for intercourse and sexual function including orgasm. During the procedure, there is direct visualization of the incision that is made at the top of the vagina into the pelvis (i.e. it is not a blind dissection like the McIndoe) nor are any tissue flaps or grafts required, nor any organs resected (i.e. bowel) to create the vagina. Simply the existing peritoneum is utilized to make a new vagina with a small incision and sutures completed laparoscopically.
Drs Miklos & Moore have been performing the Davydov procedure for almost 20 years with a > 97% success rate with one surgery and a very low complication rate. They have performed over 400 Davydov procedures and currently perform approximately 3-4 per month and have patients which have traveled more than 5000 miles for their surgery. Their complication rate is shown below.
Surgical Risks- Injury & Complication Rate</h2
Less than 1-2% bowel obstruction / ileus
Less than 1% reoperation rate
Less than 1% vaginal stenosis rate
Less than 1% Bladder injury
Less than 1% Bowel injury
Less than 1% Ureter injury
Less than 1% Blood transfusion
Less than 1% Large incision rate
Less than 1% Wound infection rate
Risks such as injury to bowel and bladder always exist however are very minimal risks with this surgery. The ureters (the tubes from the kidneys to the bladder) do run through the pelvis and these are checked closely prior to the end of the surgery to ensure that they were not kinked off by the suture placement. In Dr. Miklos and Moore’s hands they have never cut a ureter in over 400 cases (as of 2017). Risks of bleeding is minimal and the average blood loss is less than 1-2 tablespoons of blood. The chance of a post-operative infection is rare as is the risk of the vagina scarring down or shortening. The risk of vaginal scarring and shortening exist, however again with proper post-operative care, proper dilation and pelvic floor therapy, if indicated, this risk is also very minimal.
Surgery is of course only one step for young girls with MRKH and adequate pre-operative counseling should be completed and the patient and her family needs to be mentally ready for surgery and post-operative care, dilation, maintenance etc. Support groups and counseling are available for young women with MRKH and information about the condition, frequently asked questions, how to talk to your teen about the condition and other information can be found at www.MRKH.com
