Laparoscopic Sacrocolpopexy Mesh Removal
The sacrocolpopexy for the treatment of vaginal vault prolapse is the gold standard operation in the world for vaginal vault prolapse however it sometimes need to be removed due to unexpected complications. Drs Mklos & Moore have been removing these meshes for more than 20 years through either a vaginal approach or a laparoscopic approach if the whole mesh needs to be removed.
What is a sacrocolpopexy?
The sacrocolpopexy surgical procedure is the gold standard operation for the treatment of vaginal vault prolapse for more than 40 years here in the United States. The sacrocolpopexy was first introduced into the United States in the 1970s by Duke University and Dr Miklos & Moore were two of the first surgeons in the world to start doing this operation laparoscopically in 1997. This procedure was traditionally performed through a large abdominal incision and over the last 20 years has been also performed through a laparoscopic approach or using a robot. In this surgery the deepest 25% of the vagina (vaginal vault) is supported by attaching a piece of mesh to it and then suspending the mesh and the attached vagina to the sacrum (i.e. tailbone)
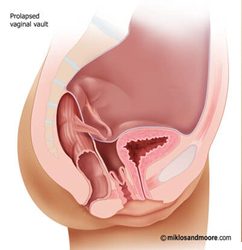 Vaginal Vault Prolapse |
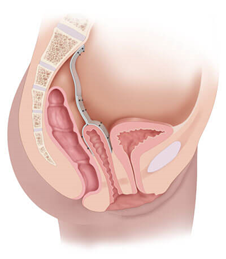 Sacrocolpopexy Support |
What are the potential mesh complications?
All surgical procedures have the potential for complications and so does the sacrocolpopexy. The sacrocolpopexy is usually performed with a polypropylene synthetic mesh throughout the world but has also been described using Gortex, Marlex or mersilene mesh as well as cadaeveric, pig or cow tissue. The safest of all mesh is the soft polypropylene synthetic mesh but it too can create complications such as: vaginal pain, lower abdominal pain, deep pelvic pain, painful sex, vaginal mesh exposure / extrusion, abscess formation, infection, bowel or bladder erosion.
Why do patients get pain from the sacrocolpopexy?
The most common reason why mesh can cause pain after a sacrocolpopexy is the tightness and pulling of the mesh (due to scar tissue) on any neighboring tissue and its associated nerves. Sometimes the pain can be due to the scar tissue created by a simultaneous hysterectomy at the apex of the vaginal vault and not due to the mesh which is in the same vicinity. No one can predict as to which patient may suffer from vaginal pain after a sacrocolpopexy.
What pain symptoms will patients report?
Patients can have pain with or without intercourse. Normally the pain is isolated to the vagina (with or without intercourse), but can be associated with defecation, urination or persistent pain in the lower abdomen or pelvis.
How is the diagnosis made that the mesh is causing pain?
Examination performed by an experienced surgeon like Drs Miklos & Moore will usually reproduce pain by touching the vagina where the mesh is attached. If pain is reproduced with touching the area where the mesh is attached this is usually indicative that the mesh might be responsible for the pain. Reproducing pain in other areas of the vagina and pelvis where the mesh is not does not rule out the mesh as the culprit if the area of mesh placement also reproduces pain with palpation.
How is vaginal mesh extrusion treated?
When mesh is coming through the skin the patient can present with vaginal pain, pain with intercourse, vaginal bleeding. This can usually be treated by resecting the mesh via vaginal approach i.e. no abdominal incisions. In experienced hands the success rate of this surgery is approximately 90% and that means one surgery and the extruding mesh is removed and the complication is cured.
What are the symptoms of a patient who has mesh erosion into the bladder or the rectum?
Mesh in the rectum can be asymptomatic (no symptoms) but more often will cause pain with defecation and blood in the stool as well as pain with sex and vaginal pain. Mesh in the bladder can also be asymptomatic but again the patient can present with pain with urination, blood in her urine, pain in the vagina, lower abdomen or the bladder
How is mesh in the bladder or rectum treated
Drs Miklos & Moore recommend complete removal of the mesh from the bladder and rectum. Mesh erosion in the bladder is best accomplished via laparoscopy and mesh removal from the rectum is repaired either laparoscopically or vaginally depending upon where the erosion is in the rectum. In bladder or rectal erosions, the mesh is removed from the organs and the hole in the bladder or rectum is closed
How is persistent mesh extrusion through the vaginal apex?
If mesh persists in its extrusion through the vaginal skin despite multiple attempts at mesh removal, sometimes the best treatment is complete removal of the mesh. Most surgeons will not attempt the removal of sacrocolpopexy mesh via a laparoscopic approach. Drs Miklos & Moore have more experience than 99% of the surgeons in the world removing mesh laparoscopically.

