The Best Hysteropexy Procedure
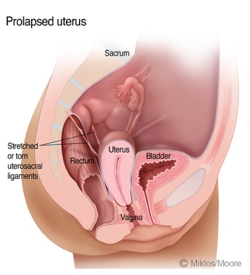
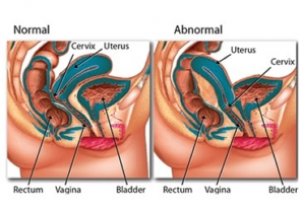
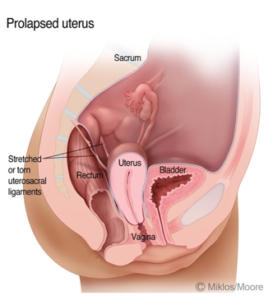
There are several different types of hysteropexy (ie Uterine suspension) surgical procedures which have been developed over the last century, however the classic sacrocolpohysteropexy remains the gold standard surgical procedure. The hysteropexy comes in many different approaches and types for the treatment of uterine prolapse, infertility and collision dyspareunia, however they all claim to accomplish the same goal ie uterine suspension. As with any surgery the hysteropexy procedures are not created equal and have differing rates of complications and cure.
Hysteropexy Types
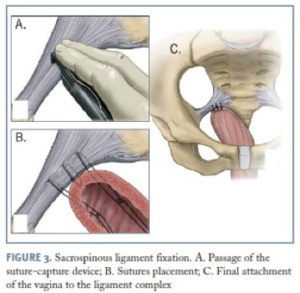
Sacrospinous Ligament Suspension– (vaginal approach) — This approach to the hysteropexy is performed through a long incision in the posterior vaginal wall of the vagina. Once the incision has been made either one or both the sacrospinous ligament must be identified and usually two sutures are placed through one or both sacrospinous ligament. Some surgeons suspend the uterus only to one ligament and others to both ligaments. The operation is considered minimally invasive because the incisions sites are hidden inside the vagina.
As with any surgery the success rate of the surgery is only as good as the surgeon performing the surgery. Failure rates of the vaginal vault as documented in the literature can range from 0-21 % within the first year. However, the sacrospinous ligament fixation also increase the rate of anterior vaginal wall prolapse after the surgery. The theory as to why this happens is that after the sacrospinous ligament suspension there is more tension on the anterior vaginal wall and it is pulled away from its supporting attachment and produces anterior vaginal wall prolapse in the form of a cystocele or urethrocele.
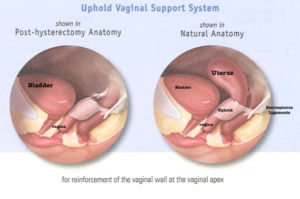
UpHold (vaginal approach using Mesh)
The UpHold is a mesh device and system produce by Boston Scientific and was designed as an anterior sacrospinous ligament vault suspension surgery. Most sacrospinous ligaments suspension surgeries are done through an incision on the posterior vaginal wall (ie floor of the vagina) instead of the anterior vaginal (ie ceiling of the vagina). The technique was designed to improve vaginal vault support. This procedure is like the sacrospinous ligaments suspension above but it uses a piece of mesh which is placed through a skin incision and attached to the uterus and the vagina and then the mesh is attached to both sacrospinous ligaments ie bilateral attachment.
One recent study supports the use of the Uphold as a supportive vaginal vault suspension procedure but it has an “overall rate of serious complications of 4.3% (9/207 patients) this included: 3 bladder perforations, 1 hemorrhage (>1000mL), 2 patients needed a reoperation due to chronic pelvic pain and 3 other readmissions for surgery due to mesh extruding through the skin of the vagina.
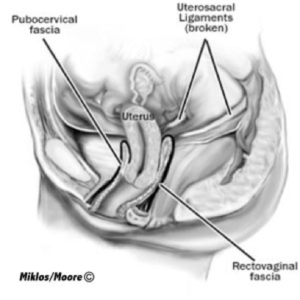
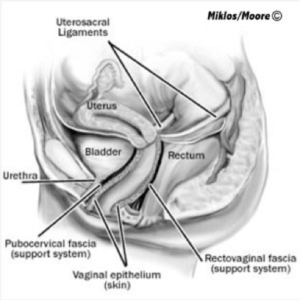
Uterosacral Ligament Suspension
The uterosacral ligament suspension operation is also known as a High McCall procedure and is the original way which Dr Miklos and Moore trained to do a hysteropexy in the 1990’s. However, the uterosacral ligament suspension has not proven to have long term cure rates and thus they have abandoned the surgical procedure.
The surgery can be performed though a laparotomy (large incision) or laparoscopically (mini incisions) by placing 2-3 sutures in both uterosacral ligaments and then sewing the ligaments to the uterus. The reason why this surgery doesn’t have a high cure rate is because either the ligaments give way or the sutures do not stay attached to the uterus. The reason why Dr Miklos & Moore will only perform this surgery (at the request of the patient) is because the cure rates are so low. It just does not hold up. However, some patients want to avoid mesh at all costs and Drs Miklos & Moore will do the surgical procedure the patient requests but only after educating the patient about the risks, benefits and complications as well as failure rate of the surgery.
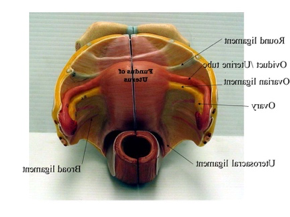
Round Ligament Suspension (Gilliam Procedure)
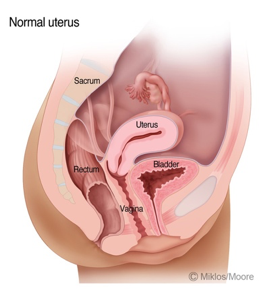
The round ligaments are not the main supportive ligaments of the uterus. Most surgeons know that the uterosacral ligaments (discussed above) and the cardinal ligaments are primarily responsible for uterine support and when these are defective the uterus prolapses.
No one has ever claimed the round ligaments is responsible for keeping the uterus from prolapsing. The round ligaments are required for maintaining anteversion and that means the fundus (top of the uterus) leans forward and into the bladder versus retroversion and leaning backwards and into the hollow of the sacrum. So, as you see they are not supportive ligaments of the uterus but instead positioning ligaments of the top of the uterus making the uterus: anteverted, midposition or retroverted. So, by shortening the round ligament the uterus is pulled forward or anteverted by lengthening the round ligament or stretching of the ligament the uterus can become retroverted or tilt backwards.
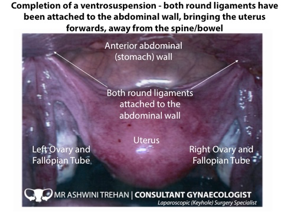
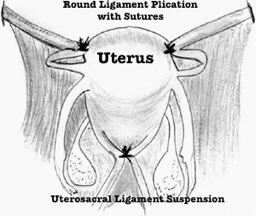
So, you can see in the first two illustrations above the round ligament is really for positioning of the of the fundus of the uterus either. However, some surgeons use the round ligament to support and suspend the uterus for uterine prolapse and this technique is known as the Gilliam procedure. The problem with this surgery, despite being around for decades, is it has never been proven to work for uterine prolapse and in theory should work better for uterine fundus repositioning.
The above medical illustration depicts the difference between round ligament plication (Gilliam procedure) versus uterosacral ligament suspension. The photo on the right depicts a Gilliam surgery as the round ligament is sutured to the belly wall to lift the uterus.
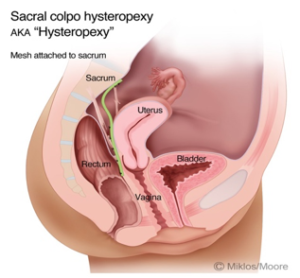
Sacrocolpohysteropexy
The word sacro (tailbone) – colpo (vagina vault)- hystero (uterus)- pexy (support) simply means support the uterus and vagina to the tailbone. This operation is also known as the sacrocolpopexy which has been in existence for more than 60 years and remains the gold standard until this day.
Drs Miklos and Moore have been trained to do all the above surgical procedures but have learned over years of experience that the sacrocolpohysteropxy or hysteropexy using mesh in their hands is the safest, most reliable and most highly curative operation known to surgeons today. In fact they are so sure of the surgical technique and cure of uterine suspension they will guarantee the surgery for 5 years. If the uterus prolapses again they will repeat the surgery for no out of pocket surgeons fee.
The cure rates of the hysteropexy using synthetic mesh as the suspension material is >95% 5 years after surgery is performed by Dr Miklos and Moore. They have performed more than 500 sacrocolpophysteropexy (with uterus) and more than 1500 sacrocolpopexy (uterus removed). The chance of a complication is as follows:
Bowel injury < 1 %
Bladder injury <1 %
Rectal injury <1 %
Ureter injury <1%
Mesh extrusion < 1/500 (Dr M & M have never experienced with hysteropexy)
Mesh infection <1/500 (Dr M & M have never experienced with hysteropexy)
Mesh erosion <1/500 (Dr M & M have never experienced with hysteropexy)
The hysteropexy with mesh supported to the sacrum is the best surgery ever developed and mesh complications are almost nonexistent. The reason? Simple the mesh does NOT come in to contact with the myofascial layers i.e. muscle and fascia, not does it penetrate myofascial layers and nor does the mesh come in contact the vaginal skin like most transvaginal mesh surgical procedures. Thus, there is less of a chance of extruding through the skin, creating painful intercourse or having an infection. Though Dr Miklos & Moore will never guarantee that a patient could not have complications of mesh they are extremely unlikely during a hysteropexy mesh procedure. Dr Miklos & Moore can also do this surgery with human, cow or pig tissue but they do not recommend these surgeries as studies have shown lower cure rates with living tissue over synthetic materials. However, it is your body and Dr M & M will respect your wishes and do the surgery the way you would like it performed (but only after a full discussion to make you an informed consumer).
- Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct2010; 2:209-16.
- Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J2013; 24:1803-13
- Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J,Vierhout ME, Kluivers KB, van Eijndhoven HWF. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ 2015;351:h3717
- Altman D, Mikkola TS, Bek Km, Rahkola-Sojsago, Gunnarsson J, Engh ME, Falconer C Pelvic organ prolapse repair using the Uphold vaginal support system: a 1 year multicenter study. Int Urogyn J 2016 Sep 27(9):1337-45.
Contact Drs Miklos & Moore’s office now for surgery in Los Angeles (Beverly Hills) CA or Atlanta GA.