Failed diagnosis – Naples, Florida.
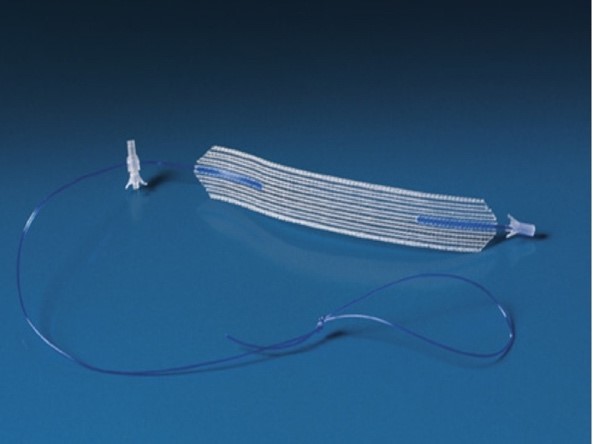
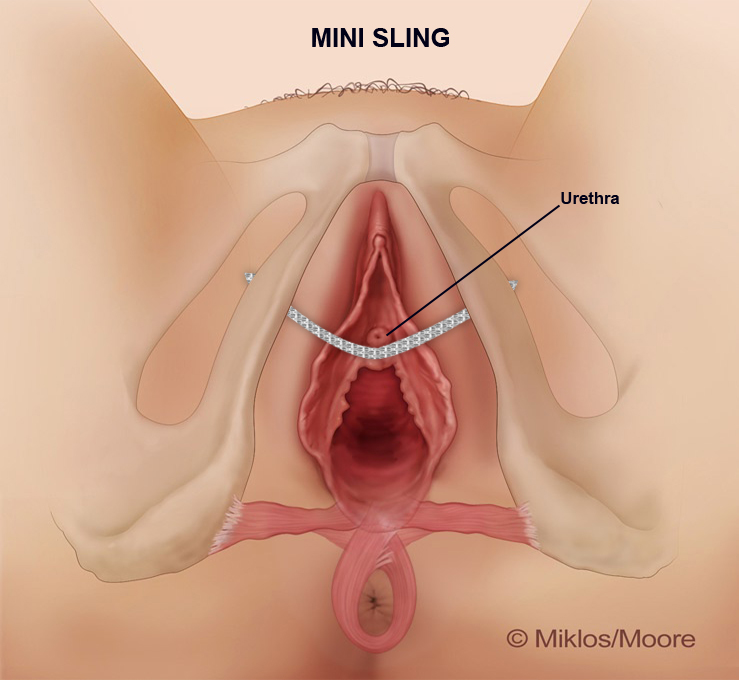
This case study focuses on a 57-year-old woman who had Laparoscopic Sacrocolpopexy (i.e. mesh) and a Coloplast Altis single incision or Mini Sling (Figure 1) for vaginal vault prolapse and stress urinary incontinence respectively in March of 2018. The Altis sling is known as a single incision sling as it only requires a single incision to place the sling underneath the skin of the urethra. (Figure 2)
Only 12 weeks after the surgery she began complaining of tension and pain in the vagina. She described the feeling of “tight” inside the vagina. She claimed that both sides of her vagina and labia, as well as her groin felt like were pulling when she walked. She also described some pain with urination at the beginning of initiating her void and at the end of the stream. She described tightness with walking (inside of the vagina), a heaviness (inside of the vagina), and claimed it was in the center. She personally felt it was the sling.
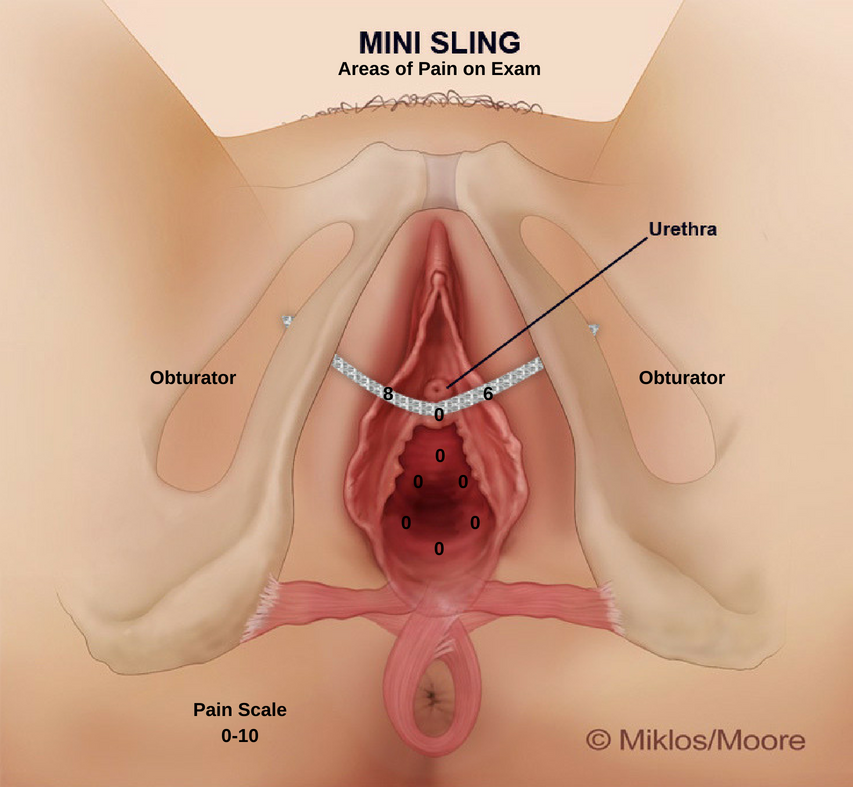
Dr. Miklos examination revealed pain in 2 of 9 areas during moderate touch during the exam. The patient was NOT informed as to what Dr. Miklos was about to touch thus limiting any bias, the severity, or presence of pain. The right side of her urethra revealed an 8/10 pain and the left side of the urethra was a 6/10 pain (pain scale + 0 -10). (Figure 3) Often patients do not feel pain directly underneath the urethra because there is little to no tension on the sling directly below the urethra. Most of the tension is lateral to the urethra and that tension is pulling on the side wall muscles known as the obturator internus. After an informed consent, the patient was taken to the operating room and the sling was removed. (Figure 4) The day after surgery her comment without provocation was: “the tension in my vagina is gone”.
No surgeon can guarantee the pain will go away with mesh removal but it is imperative if a patient is having pain to remove as much mesh as possible and as early as possible. The longer the mesh stays in the body the greater the scar tissue and the great the tension and pulling on the muscles and nerves.